Podcast interview with Pierre Robin Sequence parent
Osmosis.org is a health and medical education company that reaches nearly 500,000 health professionals, patients, and their family members. The company produces animated videos that have been viewed more than 25 million times in over 200 countries. Osmosis.org helps medical, nursing, dental, physician assistant, and other health professional students in the classroom, on board exams, and in the clinic. As part of the Osmosis.org Raise the Line Podcast series, Osmosis.org CEO Shiv Gaglani interviewed a Pierre Robin Sequence parent, Philippe Pakter.
“It’s a strange odyssey being a rare disease parent. It sort of forces you to question everything about life,” says Philippe Pakter, whose daughter Lysiane was born with Pierre Robin Sequence, a condition that impedes normal breathing and feeding. In this compelling interview with Shiv Gaglani, he shares the details of his family’s emotional, medical and legal journey. “It’s tough, but you just have to keep going, and from the hardship can potentially come very beautiful things.”
Notes
- In the interview Philippe Pakter expresses thanks to the CEO of Elsevier, Ms. Kumsal Bayazit. Ms. Bayazit worked with Philippe Pakter and helped him to publish an article on rare diseases written, from the perspective of a parent. The article was published in the Elsevier medical journal, Seminars in Fetal & Neonatal Medicine; Pakter, Philippe. “A parent’s view on the care of their baby with Robin sequence.” Seminars in Fetal & Neonatal Medicine, vol. 26,6 (2021): 101288. doi:10.1016/j.siny.2021.101288.
- In the interview Philippe Pakter mentions a physician at Stanford who administers a breakthrough non-surgical treatment for Pierre Robin Sequence in America. The physician’s name is Dr. HyeRan Choo. More can be learned about Dr. Choo and the Stanford team’s non-surgical approach in our interview with Dr. Choo.
Shiv Gaglani: Hi, I’m Shiv Gaglani. As regular listeners know, Osmosis has a special commitment to educating clinicians, patients, and families about rare diseases. In partnership with the National Organization for Rare Disorders, we’ve worked with dozens of patient advocacy groups and subject matter experts to develop nearly fifty engaging videos on rare disorders that have been viewed millions of times.
Today on Raise the Line we’re going to broaden our scope and learn about how patients and family members in Europe work with clinicians and others to advocate for themselves and their loved ones. I’m delighted to welcome Philippe Pakter, an international lawyer based in Geneva Switzerland, whose daughter Lysiane was born with a serious form of Pierre Robin Sequence. Philippe is a great example of how well-informed rare disease family members are, and why clinicians should listen closely to what they have to say.
Before we get started I wanted to thank our CEO at Elsevier, Kumsal Bayazit, who first connected me to Philippe – because actually he published his patient experience about Lysiane with some very interesting conclusions that I think are broadly applicable beyond Robin Sequence, to the rare disease community; this was in one of the Elsevier journals, Seminars in Fetal & Neonatal Medicine.
So, Philippe, thanks so much for taking the time to be with us today.
Philippe Pakter: Thank you very much, and because you brought up Kumsal Bayazit, I wanted to take a quick moment to express again my sincere thanks to her, because she reached out to me personally – having read the article that I submitted to the journal as a rare disease parent – and she granted us Elsevier’s “Gold Open Access”. And that’s just such a beautiful, meaningful gesture. We wanted as many people to read the article as possible, and by giving us open access, for us it was monumental, and I thank her from the bottom of my heart. For the people in my family and in the rare disease patient group that I am with, giving us open access on that journal article meant a lot. It really did.
Shiv: Definitely. I will say, you know, now that we’re nine months into joining Elsevier… we knew about the values, we knew about the leadership team, but certainly, they live it. They walk the walk, they don’t just talk the talk. That was just one example. I told her about our rare disease focus, and she immediately said your name, sent me your article, and connected us. So truly, a wonderful leader. I’m privileged to work for her.
So let’s go into your story. I obviously know quite a bit about you and your background. We’ve spoken a couple of times before. But for our audience, many of whom are current and future clinicians, can you just give us a breakdown of your family story about Lysiane, and your journey dealing with Pierre Robin Sequence?
Philippe: Sure. Well first of all, Pierre Robin Sequence was first studied by a French stomatologist, which is like an orthodontist, over 100 years ago, and it has three diagnostic criteria. A baby is diagnosed with Pierre Robin Sequence if the baby is showing an anatomical defect – micrognathia – which is a very small undersized lower jaw. The mandible is very small, undersized.
The second criterion is glossoptosis, which is another anatomical defect. The tongue, instead of being in a flat, horizontal position in the mouth, is in a raised vertical position, in the back of the throat. And as you can imagine, if you visualize that, that raised vertical tongue is blocking the airway, creating breathing difficulties and feeding difficulties. So that’s the second thing, glossoptosis.
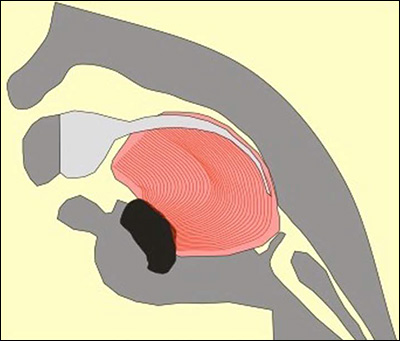
The baby’s tongue, instead of sitting flat in the mouth, sits up, in the back of the throat, in an angled or vertical position; the medical term is “glossoptosis”.
And the third diagnostic criterion is upper airway obstruction, UAO, as determined by polysomnography, by a sleep study – the baby is suffering from an apnea-hypopnea index which is above normal for a child of that age.
Now what this comes down to is that the baby is born, and the baby is struggling to breathe. It’s like you’re watching your baby suffocating, or drowning – but there’s no water anywhere around. The baby can’t breathe, because the tongue is blocking the throat. Now it’s not a strictly mechanical issue; for instance there are babies that have micrognathia which is not so severe, the lower jaw is not so small – and the tongue is not so vertical – but still, there are breathing difficulties. So it’s a complex condition, and it does have neurological components – but what it comes down to is that in the vast majority of cases, this seems to be an anatomical problem of the tongue in that raised position blocking the airway, and causing the upper airway obstruction.
Another thing is that most of the babies that are born with Pierre Robin Sequence also suffer from a cleft palate. Not a cleft lip, but a cleft palate. This is actually a consequence of the fact that during the prenatal period, the tongue, being in that raised, vertical position, prevents the roof of the mouth from fusing; fusing normally happens in the prenatal period.
The important thing to understand for medical students, and for clinicians without experience in this rare disease, is that a Pierre Robin Sequence baby is not a baby with a cleft who happens to have a small chin. A Pierre Robin Sequence baby is a baby with a complex rare disease, who happens to have a cleft – and who may not even have a cleft.
In other words, expertise in cleft care does not confer expertise in Pierre Robin Sequence. Pierre Robin Sequence is a highly complex rare disease which is still being studied, and which experts are still trying to better understand. One of the many things that separates Pierre Robin Sequence from a standard case of cleft is that the mortality rate is substantially higher. In one Dutch study, the mortality rate of Pierre Robin Sequence babies was eight times higher than the mortality rate of babies with a cleft who did not have Pierre Robin Sequence.
Another striking fact: among babies born and diagnosed with Pierre Robin Sequence, over half of these babies will also suffer from another complex associated condition; then you start talking about “syndromic” Robin Sequence, or Pierre Robin Syndrome. So you don’t just have the glossoptosis, micrognathia, and upper airway obstruction; you have all three of those, plus you have Stickler Syndrome, or Treacher Collins, or some other complex rare disease. This makes treatment that much more difficult and complex. So Pierre Robin Sequence is a heterogeneous rare disease, and it’s extremely difficult to generalize from case to case.
Unfortunately, in many situations what happens – to the detriment of the child – is that the Pierre Robin Sequence baby will fall under the care of a cleft team – which may be absolutely expert with cleft care, but which may not have a whole lot of experience with Pierre Robin Sequence. Cleft is common, but Pierre Robin Sequence is a rare disease, which only appears in approximately 1 out of 10,000 babies.
Anyway our daughter was born with Pierre Robin Sequence. Unfortunately in our case, it was not prenatally diagnosed – although it can be. By simply examining the prenatal ultrasound images, it should be possible to identify a radically undersized lower jaw. I remember that my wife, when we looked at the prenatal ultrasound images, she said to me, “Philippe, it’s kind of strange – the baby looks like Bart Simpson.” You know, Bart Simpson, from The Simpsons – he has this very small, recessed chin. And I said to her, “Look, we don’t know anything. The experts know what they’re doing, and they would tell us if something was wrong.”
But in fact the experts didn’t know. They overlooked the micrognathia, and they also overlooked another warning sign: polyhydramnios, which is a severe excess of amniotic fluid. So we’ve got two big red flags for Pierre Robin Sequence; we’ve got severe micrognathia, and we’ve got a severe excess of amniotic fluid – and no flags were raised. Nobody said, “Hey, it looks like we may be dealing with something here, maybe you should consider giving birth in a center of expertise for this rare disease, because we just don’t have a lot of experience with this.” No, it was all overlooked. This underscores the importance of a prenatal diagnosis of this rare disease, and I think the diagnosis of rare diseases in general.
Diagnosing rare diseases is not an easy thing. Many rare disease patients suffer for many years in what’s called the “diagnostic odyssey”, where you’re just waiting and waiting to find out what it is that you’re suffering from. I’ll give you an example. Lysiane was diagnosed with Pierre Robin Sequence – but she also has an another, associated condition. A genome board that was put together to study her genes, and they identified a microdeletion in one of her genes – but they’re not yet sure if this microdeletion explains her many other symptoms. Our daughter has a number of very serious developmental problems which cannot be attributed to Pierre Robin Sequence alone.
As I said earlier, in over half of the cases, Pierre Robin Sequence arises together with another associated condition. She has another condition, but they just don’t know what it is yet. So we’re in this sort of diagnostic odyssey, of waiting and hoping to find out what else she has, which is causing her other problems. I’m sorry to speak so quickly about so many different things…
Shiv: No, you’ve covered a lot. I was going to reference a couple of things you mentioned, like the importance of prenatal screening. You gave a great talk at the Third Annual Robin Sequence Consensus Meeting back in April. I’ve seen the ultrasounds of Lysiane, and you’re right, these things were missed.
One of the main points you made was that as new parents, you were kind of just trusting in the clinicians – who are doing their best – but they just may miss something, or they’re not familiar with these rare conditions. Because as we’ve shared, when you’re in med school, when I was in med school at Hopkins, the saying is, “When you hear hoofbeats, think horses, not zebras.”
The thing is, there are 7,000 zebras out there – 7,000 rare disorders that affect collectively over 300 million people. And so for those people, they don’t want the diagnostic odyssey to be four to nine years – which it is, on average – but rather as short as possible. As you said, it has real implications. If the condition is caught, you could go to a center of excellence, and get the best care. You guys in particular have a great story of how quickly you got informed, and where you’ve taken that.
Philippe: Yeah, there are very different ways that people respond to the same types of situations, in all sorts of different aspects of life. When we learned of Lysiane’s rare disease, our way of reacting was, “we need to learn everything we can possibly learn. We need to just dive in. We’re not trained, we don’t have a medical background – but we need to do our absolute utmost for our child to understand what is going on, what possibilities exist, and what the next step should be.”
Then there are parents that are so overwhelmed, so absolutely devastated, that they can experience a kind of temporary or even long-term paralysis. They just don’t know how to handle it emotionally. The way they react is that they adopt a passive role, of trusting the physicians to do what they need to do. They do not question things or attempt to get a deeper understanding; it’s just too hard, it’s too difficult.
There’s no right or wrong in this, it’s just a question of your makeup, how you react to things. We really dove in. We read everything we could. I’m American, I was born and raised in New York, so English is my first language. That was a huge advantage, because although our baby was born in France, I wasn’t doing research in French. I didn’t go to Google French. I was doing research in English – and because I was doing research in English, I successfully located a whole bunch of medical studies – which are written always in English – since English is the language which is used in international scientific research.
If you’re trying to do research in French or in Spanish or in other languages, you’re not as likely to hit the bullseye. By doing research in English, we found a number of fantastic studies coming from a certain center of excellence in a place we had never heard of before – Tübingen Germany. In Germany, Tübingen is well-known, it’s considered one of the very top universities in Germany. We didn’t know about it, but the more studies we read from this Pierre Robin Sequence center of excellence in Tübingen, the more we were convinced that this special, non-surgical treatment they offered really stood apart. It promised to resolve upper airway obstruction, and facilitate feeding – and Lysiane suffered from both of those symptoms, upper airway obstruction, and feeding difficulties. In the French ICU she was attached to a mechanical breathing machine, and also a feeding pump, which would feed her milk through a nasogastric tube.
So Lysiane needed mechanical support for two of her primary life requirements, breathing and feeding – and this treatment in Tübingen offered the prospect of addressing both of these serious symptoms, without surgery. It is an orthodontic treatment. A lot of American kids get braces, and after the braces are removed, typically the child will get a retainer – this little thing that they place in their mouth, and it just sort of keeps the teeth in the position that they’re in, in the correct position.
The Tübingen Palatal Plate, developed at the Tübingen University Hospital, is similar to a retainer. It rests on the roof of the mouth – but it also has an extension, in the back. It’s an extension which descends almost vertically, and in the back of the throat – and what that extension does is that it pushes the tongue forward and down, instantly liberating the airway.

The Tübingen Palatal Plate.
An illustration of how the Tubingen Palatal Plate works. The large pink/red object is the baby’s tongue. In the cross-section image on the left, the Pierre Robin Sequence patient has no TPP device; the abnormal rear position of the tongue blocks the upper airway, creating potentially life-threatening breathing and eating difficulties. In the illustration on the right, the TPP device is in place; it is represented by a dark blue line. The dark blue line begins at the upper alveolar ridges (where the upper front teeth will eventually grow), continues along the upper palate, covers the cleft in the palate, and then extends down. In the image on the right, toward the right side, we can see this downward dipping dark blue line extension pushing the base of the tongue left, toward the front of the mouth. By shifting the tongue forward, the TPP device instantly liberates the throat – without any invasive surgery.
So it’s like this elegant mechanical engineering solution for an anatomical defect, and it instantly liberates the airway. It may seem like, “wow, that’s pretty straightforward” – but in fact it requires enormous precision to determine the correct length and angle of that vertical extension. In the Tübingen University Hospital, that’s done with fiber optic endoscopy. A camera is sent into the airway to determine whether or not this custom made prototype of the Tübingen Palatal Plate, successfully displaces the tongue forward, and opens up the airway, for this particular baby. And it’s a question of millimeters; if the angle is off by 2 degrees, it’s no good… it’s got to be perfect, and so it requires a great deal of expertise, and a multidisciplinary team, and substantial patient volume.
So it’s essentially an orthodontic treatment, but it’s quite radical, because the Tübingen Palatal Plate promises to resolve upper airway obstruction, and facilitate feeding, without surgery. And it successfully does so, as demonstrated in 15 years’ worth of peer-reviewed medical studies.
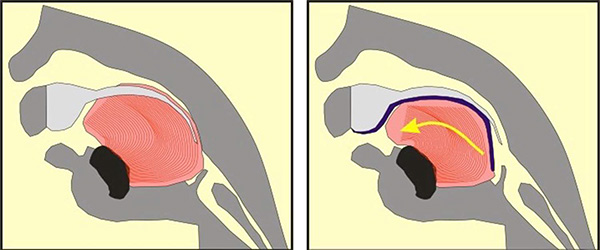
Now when you consider the other alternatives – because there are various treatments for Pierre Robin Sequence – the one that has become quite standard today, particularly in America, is MDO, Mandibular Distraction Osteogenesis. This is quite an aggressive procedure. It basically involves fracturing the mandible, the lower jaw, and inserting titanium rods. The rods have screws on them that the parents, over the course of several weeks, will turn each day, or every couple of days. This enlarges the gap between the pieces of the mandible; bone then develops to fill in the gap. So you’re actually enlarging the mandible by creating space between these two points where you’ve created the surgical breaks.
Mandibular Distraction Osteogenesis. The surgeon installs a device called a distractor, which uses special screws called “pins.”
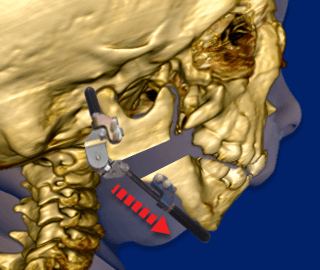
Following the initial surgery, the screws on the distractor are turned, approximately 1 to 2 millimeters per day. This creates tension, and moves the bones of the baby’s lower jaw (“mandible”) apart.
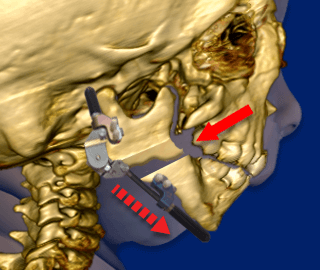
New bone then grows (“osteogenesis”) and fills in the gaps created by the distractor. While the new bone is growing, the baby continues wearing the distractor device at all times.
Mandibular Distraction Osteogenesis involves hardware, and it involves at least two rounds of serious surgery. It is supported by evidence; it generally resolves upper airway obstruction, and in the best centers, they say that it’s over 90% effective. However, the thing is that the Tübingen Palatal Plate achieves the same goals, and it doesn’t involve surgery and anesthesia.
[Editor’s note: internationally peer-reviewed medical studies relying on objective criteria demonstrate that in the vast majority of cases, the Tübingen Palatal Plate successfully resolves upper airway obstruction, without surgery; e.g. 2020, 2019, 2019, 2017, 2017, 2016, 2014, 2011, 2009, 2007, etc.]
The Tübingen Palatal Plate is a remarkable, minimally-invasive alternative to surgery. And this is a fascinating thing, because I think that while physicians may not agree on the best treatment for any complex condition – there’s always room for disagreement – I think that there are certain principles that we can all readily agree on. One of those principles that we can all readily agree on is that surgery on a newborn baby should only be performed when it’s reasonably necessary. Surgery on a newborn baby is a big deal, and not just for the baby, but for the parents as well. It’s a type of trauma to send your newborn baby into aggressive surgery.
So: surgery on a newborn baby should only be performed when it’s reasonably necessary – and in the vast majority of cases, the Tübingen Palatal Plate successfully resolves upper airway obstruction in PRS babies, without surgery. The third step in this logical progression is that surgeons that are carrying out MDO on Pierre Robin Sequence patients are, in the vast majority of cases, carrying out unnecessary surgery on a newborn baby. And that’s a heavy thing. That’s really, I think, a provocative issue that demands exploration.
One of the things that I do, along with my colleagues in our rare disease patient group for Pierre Robin Sequence, is we interview leaders in this field. It’s a small world; that’s true of all of these rare diseases. You’ve got this small group of clinicians that are really fascinated by this condition, and they develop deep expertise in it. They generally know one another, and they read one another’s studies, pre-publication, and provide comments to one another. It’s this closely knit community, international, from all over the world.
I know a good number of the physicians in the clinician community for Robin Sequence. We interviewed a brilliant physician at Stanford named Dr. HyeRan Choo. She adopted this same orthodontic approach to treating babies with Pierre Robin Sequence, and we’re doing a really wonderful interview with her that is going to be published within a week.
[Editor’s note: the interview with Dr. HyeRan Choo at Stanford University was published, and can be read here.]
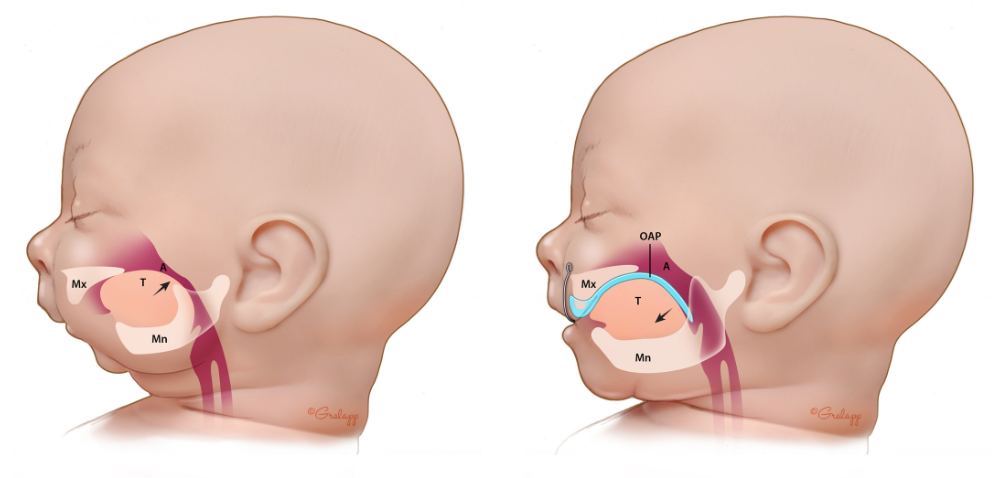
An illustration showing how the Orthodontic Airway Plate, which is administered by Dr. HyeRan Choo and her multidisciplinary team at Stanford, pushes the base of the tongue forward, toward the front of the mouth. By shifting the tongue forward, the Orthodontic Airway Plate instantly liberates the throat, without surgery.
I would love to provide a link if possible that you could include in your notes for this podcast, because the treatment has now crossed the ocean and has been adopted by Stanford in America. Also, it’s in the process of being adopted at Harvard, by another fantastic Pierre Robin Sequence expert named Dr. Cory Resnick.
Our organization did an interview with Dr. Cory Resnick last year on the prenatal diagnosis of Pierre Robin Sequence. Cory and his team have done fascinating research on how to use not only MRI, but also ultrasound, to correctly identify, with a very small margin of error, Pierre Robin Sequence – during the prenatal period. This prenatal diagnosis comes with many advantages, as we talked about before. I mean a prenatal diagnosis allows us, the parents, to mentally prepare, emotionally prepare, for the rough road ahead – but it also allows us to plan. “Let’s give birth in this hospital, or in that hospital – but definitely not at home,” you know? It allows for actual planning. It allows you to begin thinking about which team you want to choose, for the treatment of your child, who has these special needs, and so on. So that was another interview that we really enjoyed doing, on the prenatal diagnosis of Pierre Robin Sequence.
We love when physicians push the envelope, when clinicians challenge established thinking, and say, “Why not? Why not try this? This looks promising. Let’s pursue it. Let’s do some studies, let’s really explore this.” Because there is an unfortunate lack of sufficient research in rare diseases, across the board, for many complicated reasons. There are thousands of rare diseases, and they’re generally quite complex, and there is a lot of variation from patient to patient – and there are other challenges. For example, it’s tough for a pharma company to dedicate enormous investments into developing a treatment which really, at the end of the day, may have quite a small market size. You can’t argue with financial reality. I mean, it would be great if more resources were devoted to research into rare diseases. But these sorts of economic limitations result in the fact that the vast majority of rare diseases have no approved treatment or cure.
That’s one of the devastating realities which all of us rare disease patients and parents have to live with every day: 90% to 95% of rare diseases have no effective treatment or cure. So we are living day to day, week to week, month to month, in the hope that there might be some light at the end of a long tunnel. But it’s really a tough situation to be in. It’s really tough.
That’s why it’s so beautiful when we see support from the private sector, like the beautiful gesture of support from your CEO at Elsevier, when she provided us with open access for our article. We think that the article we wrote will help open the minds of clinicians that are involved in Pierre Robin Sequence, as well as students and clinicians that are still in a training period. We raised a lot of interesting questions in the article; the article is not some emotional tearjerker – “here’s what happened to us, here’s our painful patient journey.” It’s much more than that. We talk about various treatments for Pierre Robin Sequence, from the perspective of the patient. And that’s important, because you’ve got data, but you also have people, and both are key in the mix. So please read the article, whether or not you know much about Pierre Robin Sequence. I think that it will help you to see things from a slightly different angle, and that’s always helpful in life, to see things from a slightly different angle.
[Editor’s note: the article is available here.]
Shiv: Absolutely, and I’m glad you touched upon that. There’s so many threads we can pull on based on what you were just saying. I did read the article and one of the things I love about meeting people like you in the rare disease community, in general, is just how clearly passionate you are about it, because it’s your daughter. It’s your family. And this theme of partnering with patients and clinicians and researchers, all partnering – think about what would happen if patients or family members with the more common diseases, like diabetes and hypertension, took 0.01% of the motivation and passion that’s evident in so many of the rare disease community groups. We would be able to prevent so much needless suffering, and pain, and healthcare costs.
One thing I want to touch upon which you made clear in your talk, is that because it’s 1 in 10,000, or 1 in 100,000 for other rare disorders, there isn’t going to be a rare disease center of excellence for every rare disease, in every country. You make this point in your article. It’s important for governments and others to make it possible… not to hinder, but to help rare disease patients, to go to these centers of excellence, for the best care. So for instance, they’re not going to go to a cleft specialist, but they’re going to a Tübingen Palatal Plate specialist, whether that’s at Stanford, or in Tübingen.
Can you talk a bit about some of the challenges you faced? Lysiane was born in France, the treatment is in Germany. I think that with your legal background, you’re involved in getting France to pay for the healthcare costs that you and your family faced in Germany.
Philippe: I do have quite a bit of experience in this question of cross-border healthcare in Europe, which is a funny thing, because I’m an American. I learned a lot about cross-border care in Europe, particularly in the context of rare disease patients, because of this situation we faced with our daughter Lysiane.
She was born in France in a hospital which was not a center of excellence for her rare disease – and she really did need to be in a center of expertise for her rare disease. She has a syndromic form of Pierre Robin Sequence; she had and she continues to have very serious problems. France should have permitted us to transfer Lysiane to a center of expertise, and we had identified a Pierre Robin Sequence center of expertise, the Tübingen University Hospital, in Tübingen Germany. You might think, “well you’re in France, and now you’re talking about going to Germany” – but Germany is just across the border. It’s not a very long drive in an ambulance.
So we learned about the laws. I’m a lawyer, so I was able to do this legal research – and the most important law in question is called Regulation 883. This says that a patient in the European Union who has a rare disease has the right to access a rare disease treatment in another European Union country, if that treatment is not available where they live.
So we asked the French government for authorization for our daughter to receive the Tübingen Palatal Plate treatment, just across the border in Germany. We prepared a really beautiful application; it included four internationally peer-reviewed medical studies. I mean, for the Tübingen Palatal Plate, there is a controlled study dating back to 2007, and a series of medical studies after that which have looked at this treatment from every angle – and always using evidence-based medicine. For Pierre Robin Sequence, that means pre-intervention and post-intervention PSG – polysomnography exams – and weight gain data. So this is not just a bunch of clinicians saying, “We think this treatment might be effective.” This is objective criteria, really high-quality studies, put out by the center of expertise for Pierre Robin Sequence at the Tübingen University Hospital.
Well, the application was rejected by the French government. So then, what we faced was an indefinite period in the ICU. Our daughter had already spent five full weeks in the French ICU, connected to a mechanical breathing machine, and a feeding machine. Anywhere in the world, five weeks in the ICU is going to cost a fortune. So in fact we were actually saying to the French government was: “Let us save you money. Let us get Lysiane into a treatment which promises to liberate her from the breathing machine, and get her out of the ICU, in two to three weeks.” That’s it, you know? And they said no. So this wasn’t a situation where the rejection was based on exorbitant cost, for instance gene therapy – or a treatment whose efficacy or safety was in question – it wasn’t that at all. Let’s just put it this way: the rejection was not based on medical reasons.
So we were now looking at keeping Lysiane in the French ICU for another five weeks, another ten weeks, we had no idea how long it might be – because there was no scheduled date of release. The ICU had already become our second home. I mean we would go there, we would put our stuff in the lockers, we would wash our hands and arms, wear the blue gowns, and spend the whole day and evening in the ICU. Then at night we’d have to leave, we’d go home. And then we’d come back again the very next day; the daily cycle. It was very painful.
We decided, “hey, we’re going to get a bank loan.” My father actually borrowed money against his home, and he transferred the money to the German hospital – and we transferred Lysiane to Germany. We decided that the top priority was getting her into the treatment, even if we have to pay for it ourselves, because the treatment is time-sensitive. The earlier the treatment begins, the better, and the more favorably the babies respond. We thought that the legal and administrative disputes should be secondary in importance.
Well, she got the treatment in Germany. As promised, she was liberated from the breathing machine. We were out of the German hospital in, I believe, 19 days – and it changed our lives. Remember Lysiane had never left the hospital; she was born in the hospital, and she never left – five straight weeks in the French ICU, with no hope of getting out in another five weeks. We didn’t have any idea when she would get out. And so we were very pleased with the results. And then, once we were back in France, we took up the administrative appeal. And this is kind of an incredible thing, because the appeal continues to this day.
We decided to sue France in 2019 for violating EU law. We knew that Lysiane had the right to access the treatment in Germany. The European Commission specifically looked into the case, and they concluded that France was in violation. Well, we’re in August 2022, which means we have waited three years and six months – and we still haven’t had a single case hearing. So France has already violated EU cross-border healthcare law… and now France has also violated human rights law, because it is a basic human right that every person has the right to a fair trial within a reasonable time. In America we call this “due process”. But the point is that you can’t make somebody wait three and a half years without giving them a single day in court – and yet that’s what France has done. But we’re not going to give up. We don’t care if we have to fight for five years, ten years, fifteen years – we are going to get vindicated.
What all of this points to is that when a rare disease treatment is available – in the relatively unlikely scenario that there is a safe and effective rare disease treatment available – patients should be facilitated in accessing that treatment. People, administrators, and healthcare systems, should be bending over backwards to do whatever they can do to get that treatment to the rare disease patient as quickly as possible. Help the patient, by all means – why put up obstacles?
At the same time, there’s a bright side to this. The hardship we face as we seek justice for Lysiane helps to shed light on a problem that many rare disease patients face – and that problem is access to care. For rare disease patients, access should be facilitated; in practice, access is often hindered.
I would like to make a request, a sincere and heartfelt request, to the students and young clinicians that are listening to this podcast. If you face a patient with a complex rare disease, then please remember – you are probably not the best-qualified clinician to treat that particular patient. Your job is not to “fake it till you make it.” It’s not to say, “I’ve got this.” Put your confidence to the side, and just accept the fact that there is probably a clinician somewhere out there who has spent years and years studying this particular rare disease, who knows it better than anyone else – or perhaps there’s a small network of highly specialized experts on this rare disease.
Your job as a young clinician or student is to be a resource locator. You go and read the studies on that rare disease. Look at the authors whose names are popping up again and again in the literature. Reach out to those people and say, “Look, you appear to be a real expert on this condition, and I’m dealing with a patient who I believe is suffering from this condition. I’d greatly appreciate your involvement, your ideas, your suggestions, as to a care pathway. What do you say?” They’ll write back to you, because those clinicians have a passion for that rare disease, and for the patients affected by that rare disease.
So please, young clinicians, find those experts that are out there; make the connection; and help to serve as the bridge between the rare disease patient who is in front of you, and that expert who is an email away. They might be in a different state. They might even be in a different country. But it’s very likely that based on their passion, and their fascination with this rare disease, they will do more than you can imagine to help you and to help your patient. Please think of that. I beg you to think of that.
Shiv: That’s incredible advice. You put me in touch with Durhane Wong-Rieger at the Canadian Organization for Rare Disorders, and we had a chat yesterday. She’ll be on the podcast in a couple of weeks. She mentioned similar things, and suggested we make a course that basically helps our audience and early-stage healthcare professionals to not only identify these rare disorders better, but also, to do a double take on it. Hopefully, with better AI, reading these ultrasounds – and things like that – it won’t be up to them to know every rare disorder.
Being that bridge and resource is not really taught. There are rare disease communities that are lucky to have advocates like you who are intelligent, and motivated. If anyone listening to this podcast missed the intro about who you are, and what your background is, at different points they would think, “Oh, this is a physician,” based on how easily you talk about all these different conditions.” Or, “this is a parent,” when you talk about your personal journey; “this is a lawyer,” when you talk about cross-border healthcare law; “this is an advocate, leading an organization, and doing rare disease work.”
That’s an important point too. You find the right combination – of a highly motivated individual, or group of individuals – and you build the care team together. The people who are listening to this most likely are never going to see certain conditions. But the fact is that if they listen to this, of if they watched an Osmosis video on this topic – then somewhere in the back of their head, they know that there are some things that they don’t understand – and they have that humility that they don’t understand it. And they will think about being that bridge, and advocating for their patient – or having the nurse team do it, or having a social worker get trained up on how to do this. It’s really critical. I’m glad you mentioned that.
I did want to go into two other questions, and leave it open-ended. You’ve already given a lot of advice to our audience, but zooming out, what other advice would you want anybody listening to this to know about, especially when it comes to rare disease?
Philippe: I would like to encourage listeners to seriously consider exploring a rare disease, and diving in, and immersing yourself in it. These are really complex conditions. As students and young clinicians, you are all people with way above-average IQs – so it might be a really beautiful match. You’re really smart. You’re really ambitious. You’ve got this medical background – and here’s this profound mystery of a rare disease. You could become one of those global experts on that rare condition. You might find that the deeper you go, and the more you learn, the more you are loving this exploratory mission.
It can be really fascinating – and it can be discouraging – because so many of these conditions don’t yet have an effective treatment. You will see some patients come, and unfortunately, you will see them go. The mortality rate of these rare diseases is just unspeakably high, and it’s concentrated among very young patients. But that makes it more meaningful – because this is where the battle is being fought. I mean, one of the most overlooked areas of healthcare is rare diseases.
Like you said Shiv, there are thousands of rare diseases. Most of them have no effective treatment or cure. But based on what we’re learning about genetics, things could be changing. We could be turning the corner now, with gene therapy, and so you could be the one that makes a huge difference. Maybe not for the whole world, you know? Not like Jonas Salk – but for a small population of patients that desperately need help. They would be absolutely devoted to you for your efforts – for the very fact that you’re spending your time and your energy, trying to make a difference for them.
You cannot imagine the deep loyalty and devotion that we rare disease patients have for those hardcore clinicians who are at the conferences for our rare disease, and who are publishing the papers about our rare disease. We look at them as the shining hope for our children. So I would really encourage you to consider the rare disease space. It’s just an idea. The world is open for you. You can go in so many different directions – but think about this one – think about the rare disease path. It’s a worthy, worthy path.
Shiv: I think that’s beautifully articulated. It’s a story that keeps coming up… whether it’s “Chasing My Cure” [Dr. David Fajgenbaum], or John Crowley with Pompe Disease – one or more clinicians who dedicate their life to a rare disease. Whether because it’s intellectually challenging – or they have personal stories related to this condition – or they are just kind of curious about it, or want to throw a life raft out for this community that needs a lot of help.
I will say too though, as far as the Salk comparison goes, that there are examples where clinicians or researchers spend time uncovering why a rare disease happens – and there are far reaching consequences. For instance, familial hypercholesterolemia; the research behind that rare condition led to the development of statins, which are now used by over 200 million people around the world. So it’s very possible that with some of these very daunting and challenging conditions – underneath all those layers, there could be some foundational physiology or pathophysiology that could be used for many other conditions.
So I would make that clear to our audience; hopefully we can get some of them motivated to pursue this path. Two other questions. How is Lysiane doing now? She’s five years old, I think?
Philippe: Yeah, she’s five years old. She’s a handicapped child. And that’s a strange thing, because there’s this overlap between the rare disease community, and the handicapped community. She’s both. She’s got a rare disease – one that’s been diagnosed, and a second one that they are still trying to identify – and she’s handicapped. It’s quite challenging. It’s very, very challenging.
We do our best, every day. You learn a whole lot about yourself as a person, and as a parent. You are pushed in ways… you’re being forced beyond what you thought were your limits. And it doesn’t really get easier. Honestly, it doesn’t really get easier. Things change, but – it’s a strange odyssey being a rare disease parent, for us, and I think for many rare disease parents. It just sort of forces you to question everything, and ask big questions about life.
You cannot keep asking “why us?” You’ve got to shift gears and ask, “what’s next?” you know, “what’s the next step?” You don’t have the luxury of indulging in self-pity. You’ve got to meet the challenges of each day. When you’re a rare disease parent, you do everything you can for your child, to the very best of your abilities.
One of the things that we worry about – and I know that a lot of people in our situation will understand exactly what I mean – you worry about what will happen when you’re not around. How will your child be cared for, and in what way, when you’re gone? That’s one of those weird things that the typical parent doesn’t really face. You’re hoping your kid gets into an Ivy League college and gets the job that he or she wants, has a happy marriage. We actually worry about what’s going to happen when we’re dead. That seems really morbid, but it’s an example of the intense gravity of the rare disease experience – particularly when the rare disease has a neurological component – not just physical handicap, but intellectual handicap.
I mean it’s tough, it’s tough. But you just have to keep going. And I think that from the hardship can potentially come very beautiful things. In America, NORD, the National Organization for Rare Disorders – which has just been such an incredible game changer for rare disease patients in America – it was started by a woman, Abbey Meyers. She described herself – and this is a quote – she said that she’s “a simple housewife from Connecticut with children who have a rare genetic disorder.” Well, that “simple housewife” created NORD, which is responsible for the passage of the Orphan Drug Act of 1983. No policy in the world – not anywhere in America or in Europe – comes close to the benefits that have been produced by the Orphan Drug Act of 1983.
So the point is that parents without medical training, who have skin in the game – they have children with a rare disease, or they themselves are suffering from a rare disease – they can do good things. They can be meaningful parts of the movement. In the end it’s all about the clinicians, but those who are not clinicians can also contribute in a very meaningful way, and open doors for the clinicians. They can help to get research funding, they can help to push through legislation that creates incentives for pharma to invest in R&D, and so on.
And just like you said, R&D in rare disease orphan drug development often has unintended beneficial effects for the general population. When you study extreme conditions, you often learn about the more common conditions. So don’t look at it as like it’s just charity, for tiny sub-patient groups. No, it’s science – and through this research you can learn, and you can make a difference, for many many people, not just for rare disease patients.
Shiv: Absolutely. That’s such a beautifully stated example of this famous quote, “Don’t doubt that a small group of highly motivated people can change the world. Indeed, it’s the only thing that has.”
Philippe: Margaret Mead, right?
Shiv: Margaret Mead. Yeah, exactly. I paraphrased it, took a lot of liberties in that. But yeah it’s one of these quotes that’s very motivating. Whatever we can do to help raise awareness and education is something I know we’re committed to at Osmosis and Elsevier.
Philippe, is there anything else? We’ve covered a lot of ground. I’m deeply appreciative of your time. Anything else you’d like to leave our audience with today before we let you go?
Philippe: I’d like to say that sometimes physicians can feel like they’re on the hot seat. But you clinicians have one of the toughest damn jobs out there, okay? The stakes could not be higher, and there is so much that we don’t know. We know a lot, but there’s so much that we don’t know. And so I want to thank you for doing one of the hardest damn jobs that anybody can do. We appreciate you, and we need you. So keep working, and keep your faith, and please accept my thanks and admiration for your hard studies and your hard work and the stress that you face every single day, in your career as clinicians. Thank you very much. I appreciate it, and my whole family appreciates it. We do need you, and we thank you.
Shiv: Philippe, thank you so much for taking the time to share your story, and so many insights. It’s going to be very hard for us to choose the quote that goes with this podcast. And I’ll say that we’ve done over 300 podcasts; I’ve probably done about 70% of them, as the host. This is definitely one of my favorites, if not top favorite, just because I hear the passion. It has a lot of great takeaways – and I really want all of our listeners to engage in the ways you said. Whether it’s being that bridge, when they see something they don’t understand – or going all the way, and becoming a real advocate, or a leader – or attending the symposia for a specific condition – and maybe having an incredible impact from a policy perspective, or a research perspective, or a clinical perspective. Whatever they can do.
I truly, truly appreciate your time. I’m so glad Kumsal connected us.
Philippe: Thank you. Thank you, Shiv. Thank you, Osmosis and Elsevier. I really appreciate you taking an interest. I really appreciate it. Thanks a lot for this opportunity.
Shiv: Well, our listeners can expect multiple more episodes featuring rare diseases. It’s a space we’re very passionate about for the reasons we just spent the last hour discussing. With that, let me say thanks for checking out today’s show, and remember to do your part to raise the line, and flatten the curve.